Cartilage Repair
What is Cartilage?
Cartilage is the smooth, tough connective tissue that covers the ends of bones in joints like the knee, ankle, and hip. It acts as a shock absorber and allows smooth frictionless joint movement. The cartilage at the end of the bone along with the underlying bone (known as subchondral bone) together forms the osteochondral unit. The health of the subchondral bone plays an important role in keeping the overlying cartilage healthy. Cartilage is unique in the sense that it does not have a separate blood vessel that supplies it, instead deriving its nutrition from the joint fluid (also called synovial fluid). For this reason, it isn’t advisable to keep the joint immobilized for long as it can hamper the nutrition of the cartilage.
The cartilage may either suffer acute traumatic injuries (for example after knee dislocation), may get damaged due to repetitive overload mechanism (for example in patients who have recurrent dislocation of the patella), or develop ‘wear and tear’ which means age-related degeneration of the cartilage. Damage to the cartilage can lead to pain, swelling, locking, or catching of the joint along with restriction of the range of movement. The native joint cartilage is of the ‘hyaline’ type but after injury, the regenerate cartilage is of the ‘fibrocartilage’ type which is inferior biomechanically to the hyaline cartilage.
Types of Cartilage Repair Procedures:
The aim of these procedures is to prevent progression of the cartilage damage that might eventually lead to osteoarthritis of the joint.
1. Microfracture
- Small holes are made in the subchondral bone underneath the damaged cartilage
- This allows new cartilage-like tissue to form due to bone marrow stimulation
- Suitable for smaller cartilage defects
2. Autologous Chondrocyte Implantation (ACI)
- Cartilage cells are harvested from the patient’s knee from a location that doesn’t contribute to weight-bearing
- The cells are cultured and multiplied in a lab for around 6 weeks
- The new cartilage cells are implanted into the cartilage defect to cover the area of cartilage loss
3. Osteochondral Autograft Transfer (OATS)
- Plugs of healthy cartilage and bone are taken from a non-weight-bearing area of the joint
- These plugs are transplanted into the cartilage defect in the same setting
4. Osteochondral Allograft
- Cadaver cartilage is used instead of the patient’s own tissue
- Fresh or cryopreserved grafts can reconstruct larger defects
- Allograft sources have limited availability in India
What patient can expect before surgery?
- They have detailed clinical examinations to identify the nature of the pathology and recognise the presence of other associated injuries if any. Cartilage lesions of the knee are frequently also associated with meniscus tears. Functional scoring of the patient is also done at this stage, which allows for comparison with scores in the postoperative period.
- X-ray of the joint to ascertain the degree of joint space narrowing, and the presence of additional arthritic changes like osteophytes.
- A standing scannogram (special alignment X-ray) is done for cartilage injuries of the knee because Abby’s planned repair procedure may fail if there is a native abnormal alignment.
- MRI to recognise the extent and depth of the cartilage defect and also identify additional injuries.
- CT scan may be required in some patients to better understand the rotational alignment of the limb which cannot be determined on the scannogram.
- Preoperative physiotherapy assessment to assess the muscle strength and range of motion and to start “Pre-hab” exercises
- Anesthesia checkup to recognize potential medical issues that can affect the peri-operative course
- Additional investigations like blood tests, chest Xray, electrocardiogram (ECG), or any other test as determined by the anesthetist/physician as being essential for surgery
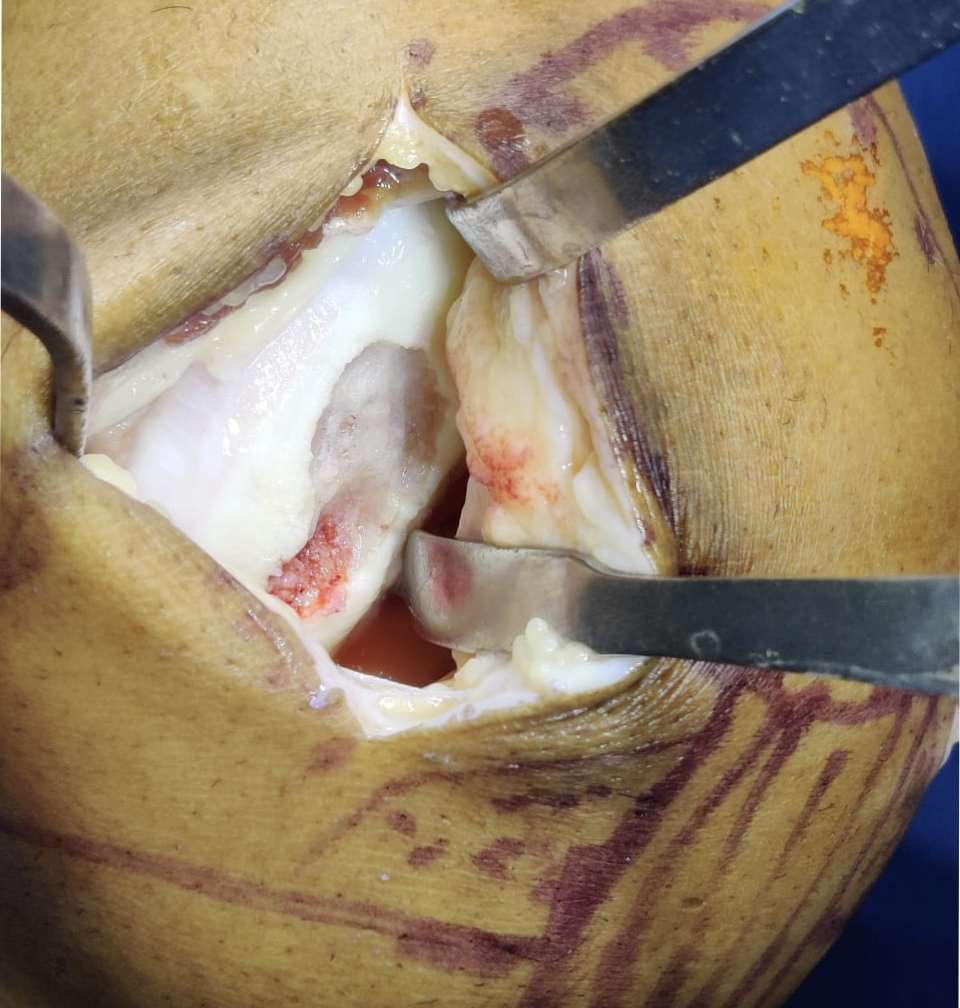
The Procedure
The surgery is usually done under spinal anesthesia that may be augmented using an epidural pump
- Done arthroscopically through small (keyhole) incisions
- The arthroscope (camera) is inserted to recognize the defect as well as the presence of additional pathology if any
- The cartilage defect is cleared of loose debris and prepared for the definitive procedure
- The planned repair amongst the ones mentioned above is performed
- Sometimes cartilage surgery is combined with meniscus repair or correction of limb alignment because these problems often coexist and performing only isolated cartilage repair in such cases can lead to premature failure
- Incisions closed with stitches/steri-strips
Recovery and Rehabilitation:
- Period of non-weightbearing and use of crutches for the first 4-6 weeks.
- Physical therapy to regain mobility and strength is allowed during this phase
- Gradual increase in functional activities from 6 weeks onwards which include low-impact activities till 4-6 months as healing allows
- Full recovery including return to sports often takes 9-12 months or more