Arthroscopic Rotator cuff repair
What is the Rotator Cuff?
The rotator cuff is a group of four tendons and muscles that surround the shoulder joint, holding the ball of the upper arm bone (humerus) in the shoulder socket (glenoid) and enabling you to lift and rotate your arm. Although the muscles comprising the rotator cuff are relatively small sized, the serve to maintain the congruency of the glenohumeral (shoulder) joint and allow the larger muscles such as the deltoid to carry out movements.
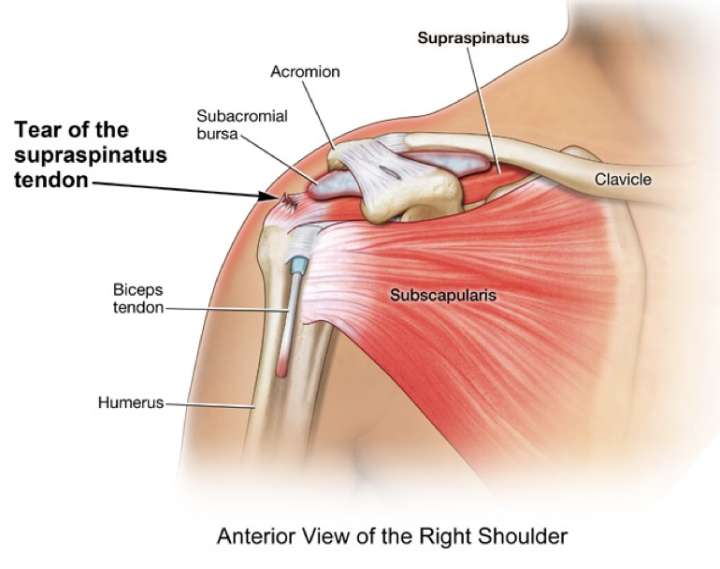
Rotator Cuff Tears
A rotator cuff tear is a common injury, often due to degeneration from overuse or aging, but can also occur from acute trauma such as a fall. Symptoms include shoulder pain, weakness, stiffness, and limited range of motion especially significant restriction of overhead activity. Often the patient is unable to lift his/her limb, a condition called as “pseudo-paralysis”. The pathology may present anywhere along a wide spectrum that ranges from degeneration of tendon (“tendinosis”) to complete tears. Patients with long standing rotator cuff tears are at risk of developing Rotator cuff arthropathy where the humerus head subluxes (migrates) superiorly and develops arthritic changes. With advanced age and poor structural quality of the aging tendon, the tears maybe massive in configuration. Some tears that are large in size may require augmentation with biological tissue, a procedure known as superior capsular reconstruction.
Arthroscopic Rotator Cuff Repair
For many rotator cuff tears, arthroscopic surgery is recommended to reattach the tendon to the bone. This minimally invasive procedure uses tiny incisions and an arthroscope (camera) to view and repair the torn tendon.
What patient can expect before surgery?
- Detailed clinical examination to recognize the meniscus tear and presence of additional pathologies if any. Functional scoring of the patient is done which is repeated after surgery at followup visits.
- X-ray of the knee to evaluate the condition of the bone and the joint
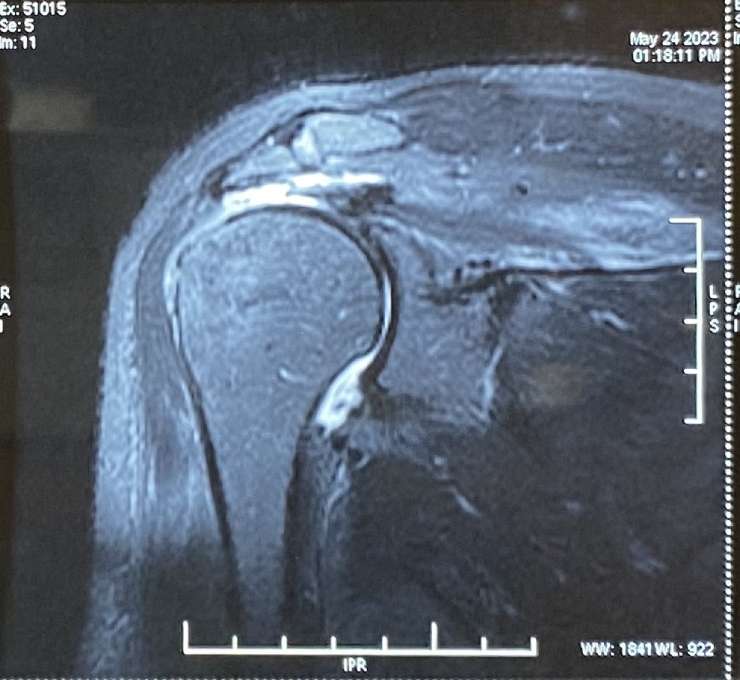
- MRI of the knee to confirm the diagnosis of the meniscus tear and also to identify additional injuries to the knee
- Some patients may require a standing scannogram which is a special X-ray done to evaluate the alignment of the lower limb. Some patients with abnormal alignment are at higher risk of suffering from meniscus tears due to overloading of one compartment of the knee.
- Preoperative physiotherapy assessment to assess the muscle strength and range of motion and to start “Pre-hab” exercises
- Anaesthesia checkup to recognise potential medical issues that can affect the peri-operative course
- Additional investigations like blood tests, chest Xray, electrocardiogram (ECG) or any other test as determined by the anaesthetist / physician as being essential for surgery
The Procedure
The procedure is generally done under general anesthesia augmented with a regional anesthesia block.
- Small incisions are made in the shoulder area.
- The arthroscope is inserted to visualize the rotator cuff tear.
- Surgical instruments are used to remove any bone spurs and repair the torn tendon.
- The tendon is reattached to the bone using sutures or suture anchors.
- Double-row repair and single-row repair are surgical techniques defined by the configuration of the sutures.
- The incisions are closed with surgical tape or stitches.
Benefits of Arthroscopic Repair
- Smaller incisions, less pain
- Quicker recovery and return to activities
- Advanced arthroscopic techniques allow the repair of larger tears
Recovery and Rehabilitation:
A phased rehab protocol is designed by the therapist that is tailored for each patient. Effective postoperative rehab is essential to maximise outcome. Early rehab focuses on restoring the mobility of the shoulder while allowing the repaired tendon to heal. Later phases of the rehab protocol focusses on maximising strength and regaining function. Physical therapy is crucial to regain strength and range of motion through exercise progression over 3-6 months. Driving and return to activities depends on the size of the tear and healing progress.