Orthopedic Surgery
Anterior Cruciate Ligament Reconstruction
The anterior cruciate ligament (ACL) is one of the major stabilizing ligaments in the knee joint. It is one of the two cruciate ligaments present within the knee joint that provide anteroposterior stability to the knee. ACL injuries are common, especially in athletes who play sports that involve sudden stops, jumping, or changes in direction. Patients suffering from a torn ACL complain of instability (or sudden giveaway of the knee) especially while walking on an uneven surface. ACL injuries with symptomatic instability, if ignored, increases the risk of meniscal or cartilage (chondral) injuries. An ACL tear often requires surgical reconstruction to restore knee stability and function.

Arthroscopic ACL Reconstruction:
Arthroscopic ACL reconstruction is a minimally invasive surgical procedure that involves replacing the torn ACL with a graft (tissue taken from the patient’s own body). The surgery is performed through small incisions (“Key-hole”) around the knee, and an arthroscope (a tiny camera) is used to visualize the inside of the knee joint. Specialized instruments allow for the procedure to be completed through small incisions. Minimally invasive techniques facilitate faster post-operative recovery. The various graft options include hamstring tendon graft, central quadriceps tendon, bone-patellar tendon-bone graft, and peroneus longus graft. Single-bundle and double-bundle reconstruction are two different surgical techniques used to reconstruct the ligament. Additional augmentation of the reconstructed ACL can be done using FiberTape which is described as Internal bracing.
What patient can expect before surgery?
- Detailed clinical examination to recognize the ligament deficiency and presence of additional pathologies if any. Functional scoring of the patient is done which is repeated after surgery at follow-up visits.
- X-ray of the knee to evaluate the condition of the bone and the joint
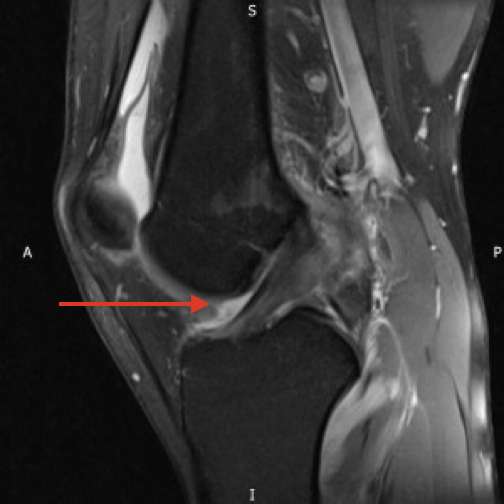
MRI of the knee to confirm the diagnosis of ACL tear and also to identify additional injuries to the knee. - Some patients may require a standing scannogram which is a special X-ray done to evaluate the alignment of the lower limb.
- Preoperative physiotherapy assessment to assess the muscle strength and range of motion and to start “Pre-hab” exercises.
- Anesthesia checkup to recognize potential medical issues that can affect the peri-operative course.
- Additional investigations like blood tests, chest X-rays, electrocardiogram (ECG), or any other test as determined by the anesthetist/physician as being essential for surgery.
Procedure:
The surgery is usually conducted under spinal anesthesia or under general anesthesia.
- Graft Harvesting: A tendon graft is harvested from the patient’s own body (such as the patellar tendon or hamstring tendons).
- Arthroscopic Visualization: The surgeon inserts the arthroscope and other small instruments through the key-hole incisions to visualize the torn ligament and identify if any additional pathology (like a meniscus tear) is present.
- Graft Preparation: The graft is cleared of all redundant tissue, and prepared for passage. It is also sized appropriately.
- Tunnel Creation: The surgeon creates small tunnels (bone tunnels) in the femur (thigh bone) and tibia (shin bone) to accommodate the new graft.
- Graft Fixation: The graft is passed through the bone tunnels and secured in place using screws and other fixation devices like an adjustable loop or fixed loop or suture disc.
- Closure: The incisions are closed with sutures or surgical staples.
Patients with high-grade instability may be candidates for Lateral extra-articular tenodesis (LET) where an additional soft tissue restraint is created on the outer aspect of the knee to further enhance the stability.
Recovery and Rehabilitation:
After the surgery, patients typically wear a knee brace and use crutches for a period of time. Generally no bed rest is required and patients are made to stand and walk with help of support from the next day. Modern anaesthesia protocols allow for comprehensive pain control and patient comfort. Physical therapy is essential to regain strength, flexibility, and stability in the knee joint. Recovery time varies, but most patients can return to light activities within a few months and more strenuous activities within 6-12 months, depending on their progress and the specific sport or activity. Patients who do not participate in any cutting/pivoting activities or those with sedentary lives usually can resume their vocational activities after 1 month. A tailored rehab program that is focused on achieving predetermined targets (goals) for each phase is designed by the therapist for each patient.