Introduction
Pelvis and acetabulum fractures are significant injuries that can affect your mobility and quality of life. The pelvis is a ring-like structure of bones at the base of your spine, and the acetabulum is the socket in your pelvis that holds the head of your femur (thigh bone), forming the hip joint. Both these bony structures are located deep within the body hence any break is often secondary to high-energy trauma which might lead to injury to additional body parts such as the head, chest, and abdomen. Similarly, these patients may also have concomitant fractures in the upper or lower limb requiring surgical attention.
Anatomy of the Pelvis and Acetabulum
The pelvis consists of three bones: the ilium, ischium, and pubis. These bones are connected to the sacrum (the base of the spine) and form the pelvic ring. The acetabulum is a concave surface (Socket) where these bones converge, creating a deep cavity that articulates with the femoral head.
Causes of Pelvic and Acetabular Fractures
These fractures typically result from high-energy trauma, such as:
- Motor vehicle accidents
- Falls from significant heights
- Crush injuries
In elderly patients with weaker bones, fractures can occur from lower-impact events like minor falls.
Symptoms
Common symptoms of pelvis and acetabulum fractures include:
- Severe pain in the hip, groin, or lower back
- Difficulty or inability to move the lower limb and walk or bear weight
- Swelling and bruising in the hip area
- Numbness or tingling in the groin or legs (due to nerve involvement)
- Both these fractures can lead to significant internal bleeding that can compromise the hemodynamic status of the patient and require intensive care
What patient can expect before surgery?
- Clinical examination to recognise the injury and presence of any additional injuries that require treatment
- Primary stabilisation of the patient is a multi-disciplinary process that aims to ensure that the injured patient is adequately treated for all additional injuries especially head/chest/abdomen/spine and pelvis injuries. Some patients may require admission/transfer to the intensive care unit (ICU) for optimisation
- X-ray to evaluate the fracture configuration and extent
- A CT scan may be required to understand the fracture configuration in some patients better
- Preoperative physiotherapy assessment focuses on ameliorating secondary complications like bedsores, pulmonary embolisms (blood clots) etc.
- Anaesthesia checkup to recognise potential medical issues that can affect the peri-operative course
- Additional investigations like blood tests, chest Xray, electrocardiogram (ECG) or any other test as determined by the anaesthetist/physician / other medical specialists as being essential for surgery
- Patients who suffer high-energy injuries often require a multidisciplinary approach involving the physician, general surgeon, plastic surgeon, anaesthetist and other allied medical fields.
- If required some patients may require to be started on blood thinners (anticoagulants) because patients with lower limb fractures are at a higher risk of developing blood clots within the circulation which may then migrate to the heart or the lungs and cause perioperative complications.
Treatment Options
Treatment depends on the fracture type, location, and patient health:
1. Non-Surgical Treatment:
Undisplaced fractures may rarely be amenable to nonoperative treatment. This requires a period of bed rest with or without other assistive devices like a pelvic binder or lower limb traction.
- Rest and Activity Modification: Initial rest followed by a gradual increase in activity.
- Pain Management: Medication for pain relief.
- Physical Therapy: In the early period this focuses on chest physiotherapy and simple precautions to avoid pressure sores. Once the fracture shows signs of union, additional exercises to improve strength and mobility can be started.
2. Surgical Treatment:
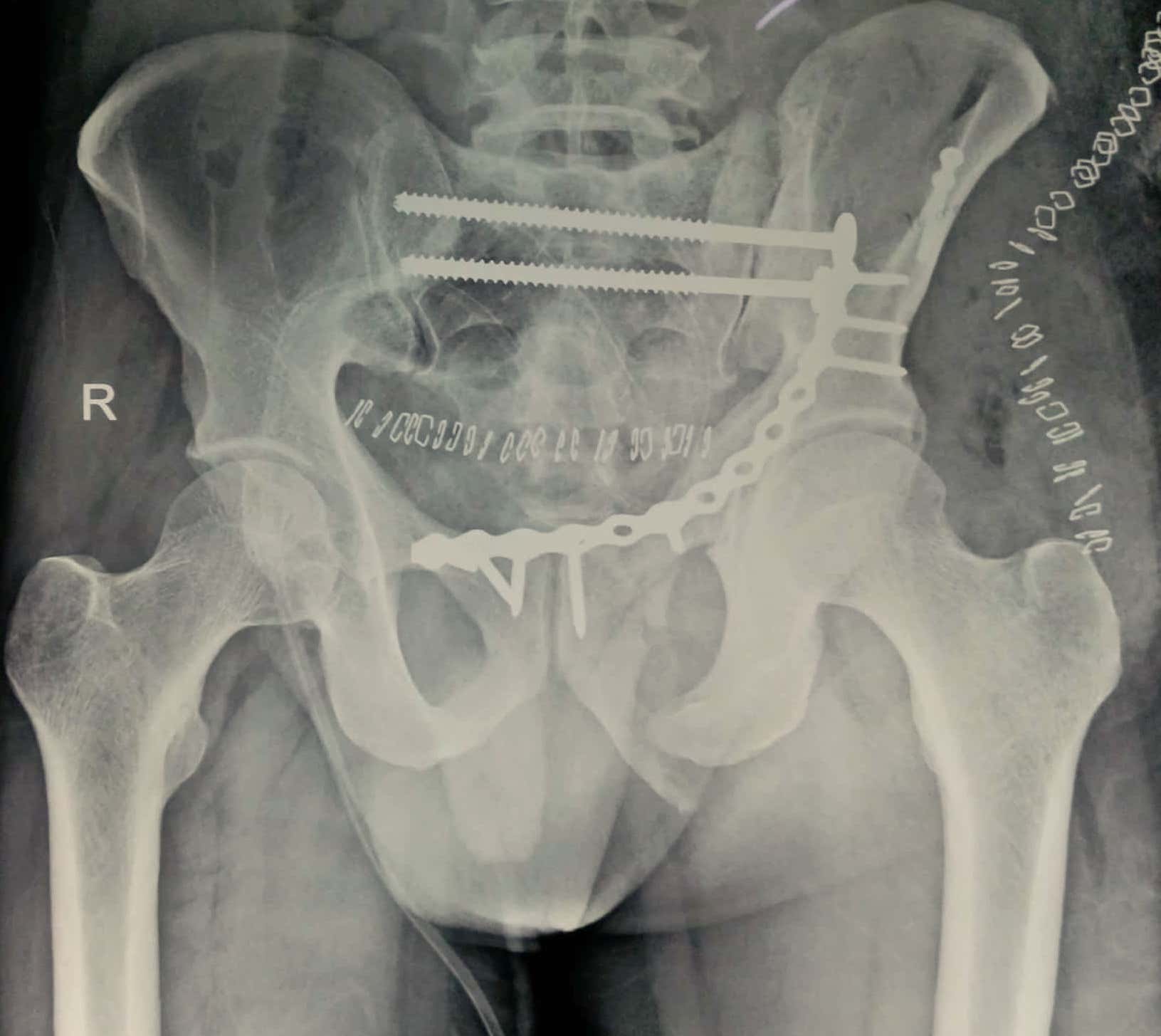
Depending upon the fracture, the surgical procedure required may be minimally invasive screw fixation or open reduction with the application of plate and screws. Sometimes both may be needed in the same patient. Surgeries of the pelvis and acetabulum are often extensive procedures requiring specialized skills and tools.
- Internal Fixation: Using screws, plates, or rods to stabilize the fracture.
- External Fixation: External devices to hold the bones in place during healing. May be needed as a temporary procedure to provisionally hold the fracture reduced till the patient is stable for definitive fixation
- Joint Replacement: In some fractures involving the acetabulum, a hip replacement may be necessary after evaluating the age of the patient and the nature of the bony injury.
Recovery and Rehabilitation
Recovery can take several months and involves:
- Follow-Up Visits: Regular check-ups to monitor surgical wound healing and bony union.
- Physical Therapy: To restore strength, flexibility, and range of motion.
- Lifestyle Modifications: Temporary use of mobility aids (crutches, walkers) and avoiding high-impact activities.
Complications
Potential complications can include:
- Infection
- Blood clots
- Nerve or vascular injury
- Post-traumatic arthritis
- Hip dislocation
The treating surgeon will discuss these in detail before surgery
Prevention
While not all pelvic and acetabular fractures can be prevented, reducing risk factors can help:
- Fall Prevention: Especially in the elderly, through home safety modifications.
- Bone Health: Adequate calcium and vitamin D intake, and regular weight-bearing exercise to strengthen bones.
- Safety Measures: Use of seat belts and proper protective gear wherever indicated.
Conclusion
Pelvic and acetabulum fractures are serious injuries requiring prompt and appropriate treatment to ensure optimal recovery. If you suspect you have sustained such an injury, seek immediate medical attention. With proper care and rehabilitation, many patients can regain their pre-injury level of function and return to their daily activities.
For more personalized advice and treatment options, please schedule a consultation.