When are the sutures removed after the surgery?
Suture removal is done at 2 weeks from the date of the surgery. Certain surgical procedures can also be done in a stitchless manner where special self-dissolving suture material is used on the surface of the skin that does not require removal. Discuss with your orthopaedic surgeon whether your procedure can be done in a stitchless manner.
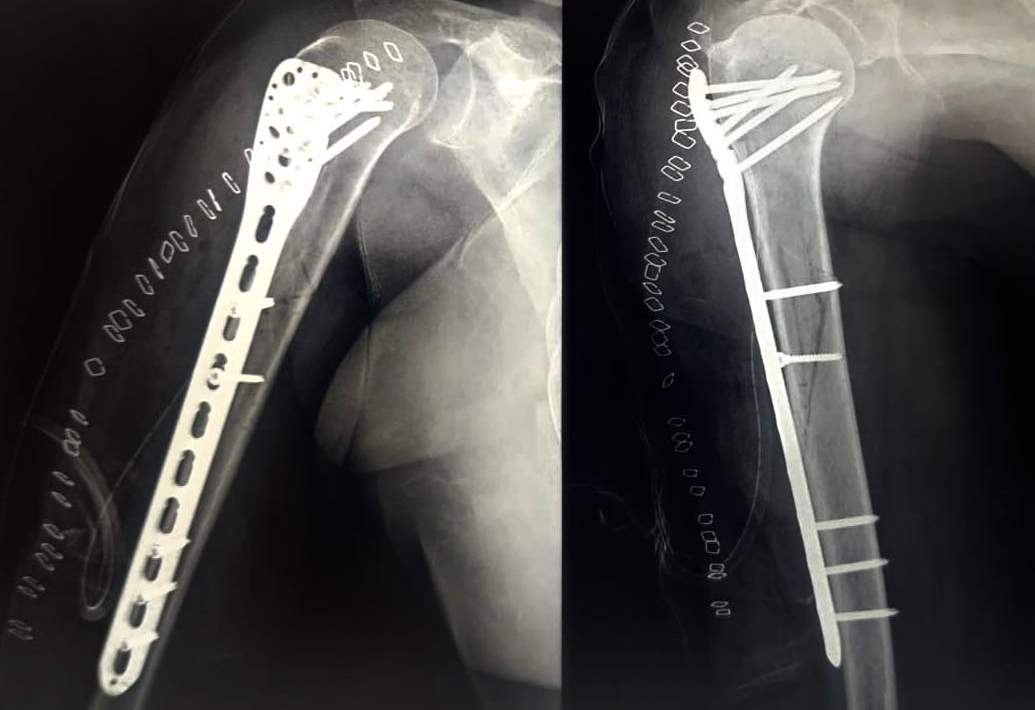
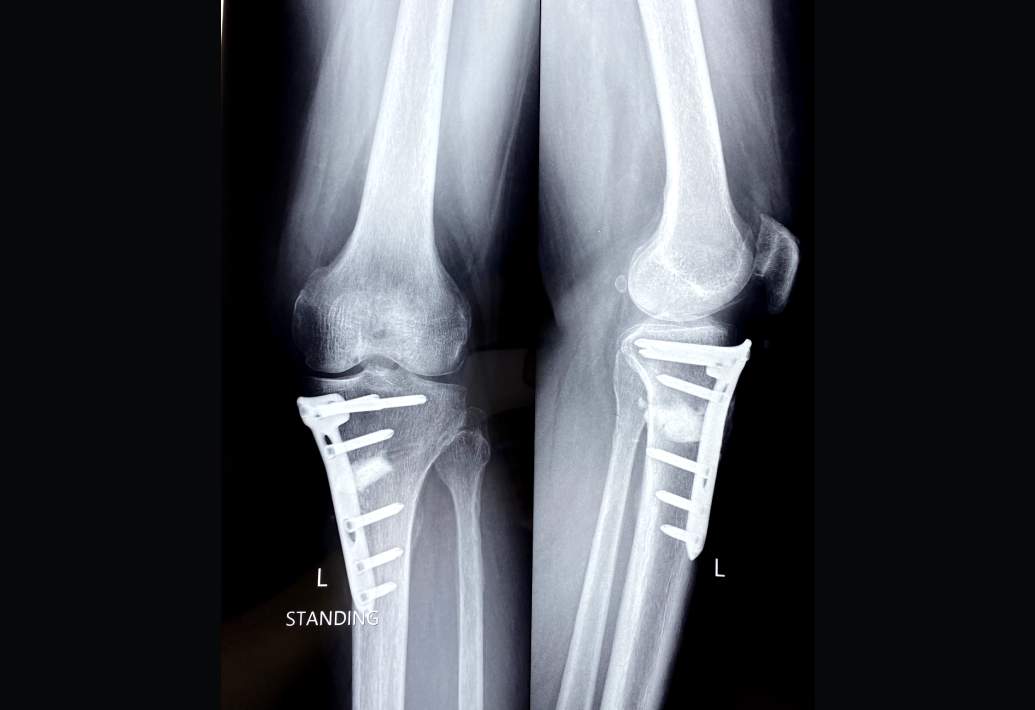
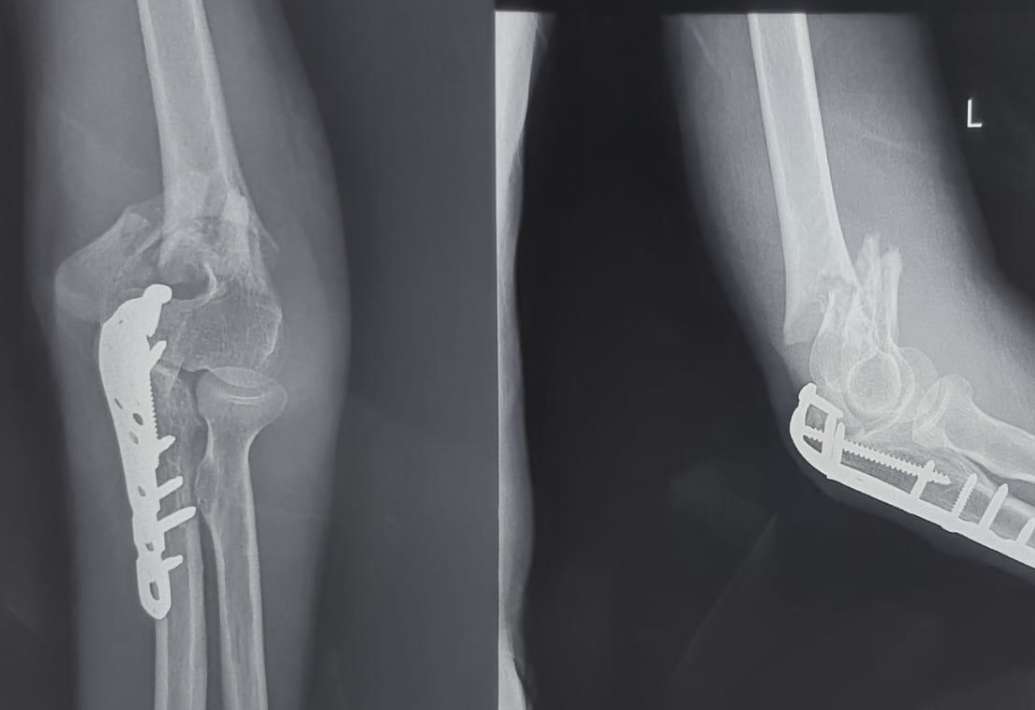
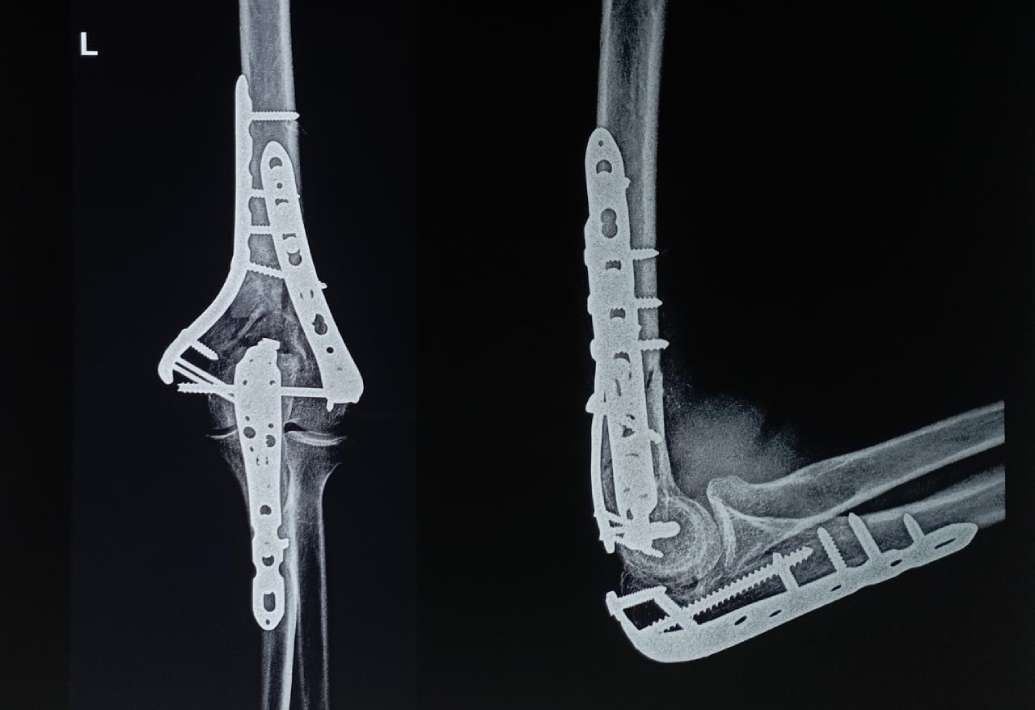
I have had a surgery done for my fracture and have am implant in situ. When should I consider implant removal.
Implant removal can be safely removed around 1 year after the index surgery. Usually a repeat X-ray or sometimes even a CT scan us required at the time of implant removal to verify the bony union. Implant removal surgery necessitates the same incision and same approach as the first procedure but will much faster post operative recovery. It is important to note that in some cases their is bone overgrowth on the screw heads which makes the removal of the screw difficult. The risk of screw breakage, inability to remove implant without risking bone injury and risk of fresh fracture during implant removal must be borne in mind. For these reasons, implant removal if desired is ideal within first 1-2 years after surgery and generally can be safely avoided if many years have elapsed. Modern Orthopaedic implants (Titanium) are biologically inert, MRI compatible and generally do not lead to any issues in the long term. Consult your Orthopaedic surgeon if planning for an implant removal.
When can I resume my job following my surgery?
This depends both upon the nature of the job and upon the surgery performed. For patients engaged in vocations that are strenuous such as machine operators, oil rig workers, trekkers etc generally requires improved muscle strength before resuming their profession. On the other hand officer goers or people who have a desk job can usually return to work around 1 month after surgery. Sometimes a walking stick/ cane or some form of splint maybe worn to the workplace in the initial convalescence period. Replacement surgeries allow return to work after 2-4 weeks if adequate strength and mobility is present. Fracture fixation surgeries have variable return to work with nailing procedures generally improving faster than plating. Arthroscopic procedures also have quicker recovery due to the minimally invasive nature of the procedure. Return to sports or athletic activities has to be placed in consultation with the treating surgeon and the physical rehab specialist.
I am on certain tablets for my medical issues, should I be worried about any potential interactions with Orthopaedic medications?
It is imperative to inform your Orthopaedic surgeon regarding the medications you are taking. This is especially true for certain types of tablets such as blood thinners (eg : Tab Clopidogrel) because they need to be withheld prior to the surgery. Similarly also inform the treating surgeon regarding any allergies to medications such as sulfa allergy. Majority of the commonly prescribed Orthopaedic medications are compatible with the treatment regimens of common medical disorders like hypertension, diabetes, heart disease etc. Your Orthopaedic surgeon will discuss with you in case any modification is needed depending upon your existing tablets.
When can I take a bath after my surgery?
The surgical wound should not be directly exposed to water till the sutures or staples are in place. Usually once the sutures/staples are removed at 2 weeks then normal bathing can be commenced. Meanwhile sponging or assisted bathing is advised to maintain hygiene. Commercially available plastic wraps can be used to isolate the operated limb for bathing purpose.
How to position the operated limb at night?
Following surgery the operated limb must be kept elevated over a pillow or special bolster so as to avoid excess swelling. Hyper elevation is not recommended and usually keeping one or two pillows underneath the operated limb should suffice.
Is cashless facility available?
Yes, cashless treatment is possible at partner hospitals.
How much pain would be there following the surgery?
Modern anaesthesia follows the principle of multi modal analgesia which means multiple pain control methods are combined to ensure comprehensive pain control. Pain controlled analgesia (PCA) allows for the patient to control the dose of the analgesic based on the pain. Preoperative as well as post operative nerve blocks minimise pain. Intra venous analgesics are given for first 1-5 days and combined with oral tablets for breakthrough pain. Transdermal analgesic patch which can be directly applied to the skin allows for comprehensive coverage. The treating Orthopaedic surgeon along with the anaesthetist will discuss various pain control options with you throughout the duration of your stay in the hospital.
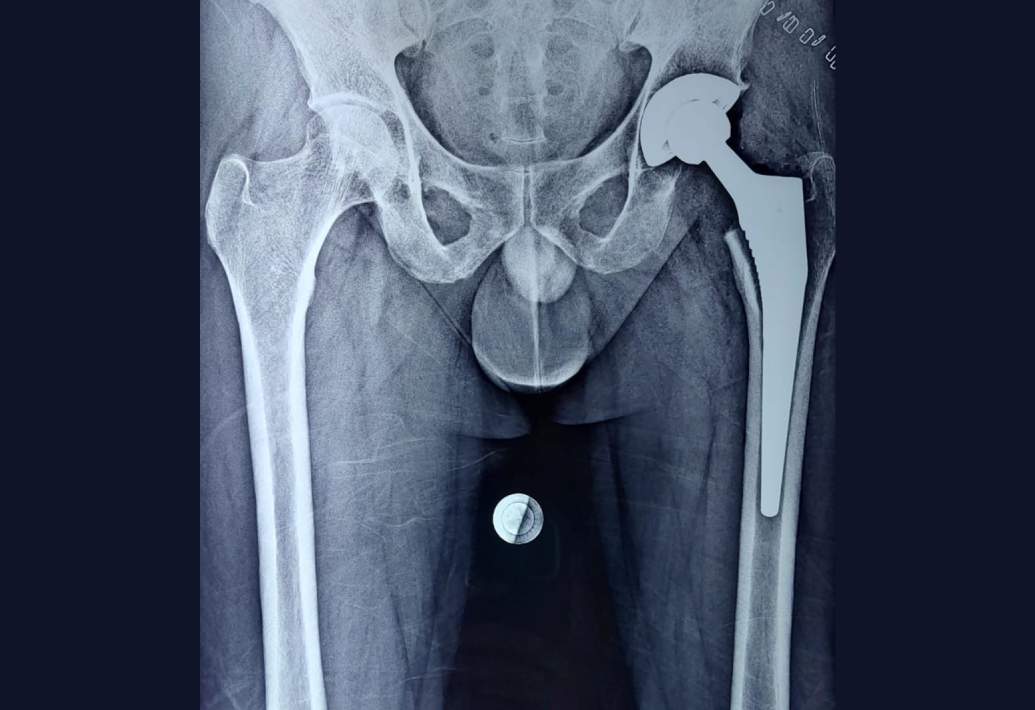
How long do the implants used in knee or hip replacement last?
The longevity of modern knee and hip implants is usually around 20 years. It also depends upon the level of activity of the patient. Vigorous activity can cause the prosthetic liner to wear out faster. These patients require a revision or redo replacement.
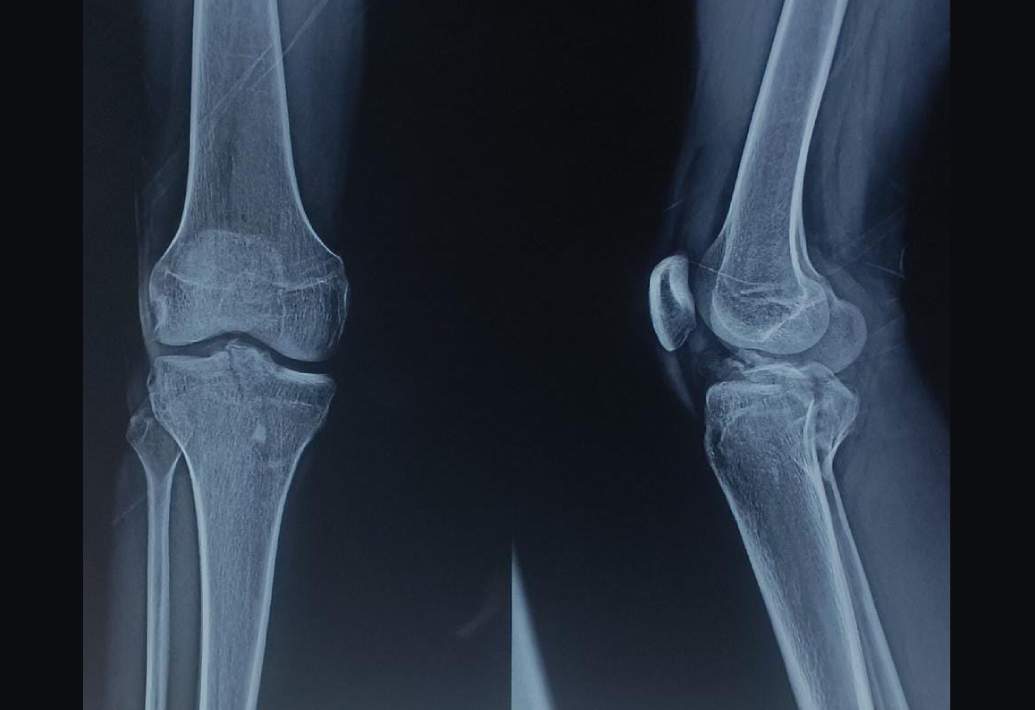
I have been advised partial meniscectomy for my knee. Will removal of the meniscal tissue affect my knee function?
Partial meniscectomy is advised for tears that are deemed irreparable either due to the complexity of the tear with multiple flaps and fragile tissue quality or due to the location of the tear within the avascular (White-White) zone. Patients with such tears suffer from frequent locking, recurrent swelling and pain due to the torn meniscal fragments getting interposed within the tibia-femoral joint space. Frequent locking aggravates the risk of developing cartilage damage and this can best be prevented by removing the meniscal tissue which is responsible. The entire meniscus is not removed and a stable meniscal rim of healthy tissue is left behind at the end that continues to serve the function of the meniscus.
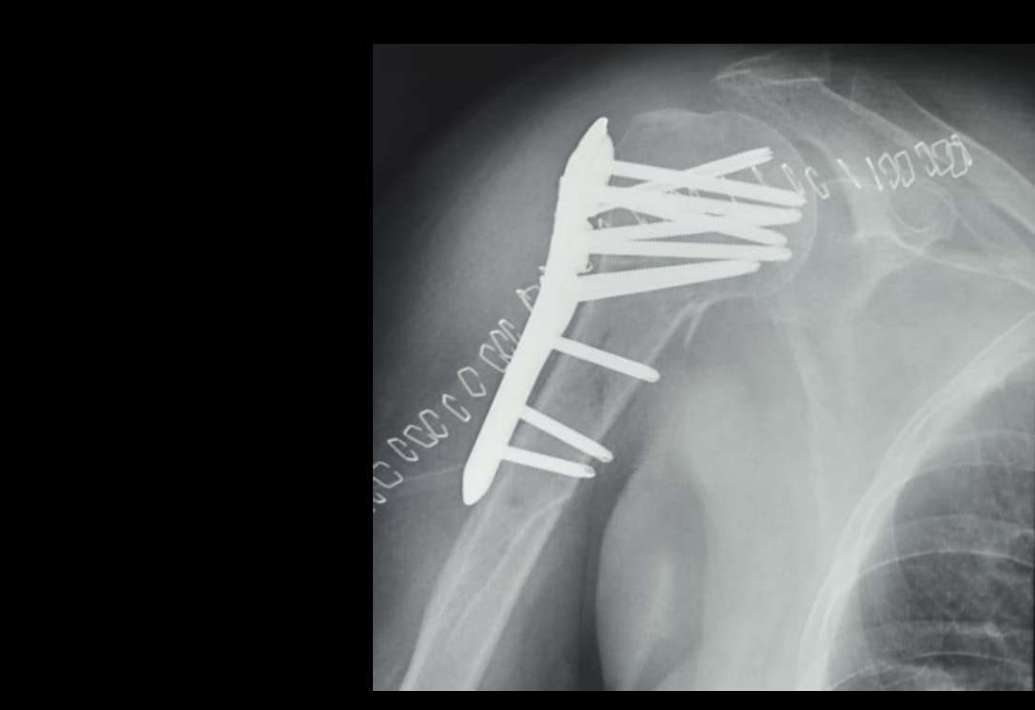
What is the material of the metal plate/screws or the metal nail used for fracture fixation?
The orthopaedic implants used in fracture fixation are either made of stainless steel or titanium. Stainless steel alloys designated as ASTM F-55 and ASTM F-56 (grades 316 and 316L) are used amongst the various alloys of commercially available stainless steel. Titanium-aluminium-vanadium alloy (ASTM F-136) also referred to as Ti6AI4V is the titanium alloy used to manufacture implants.
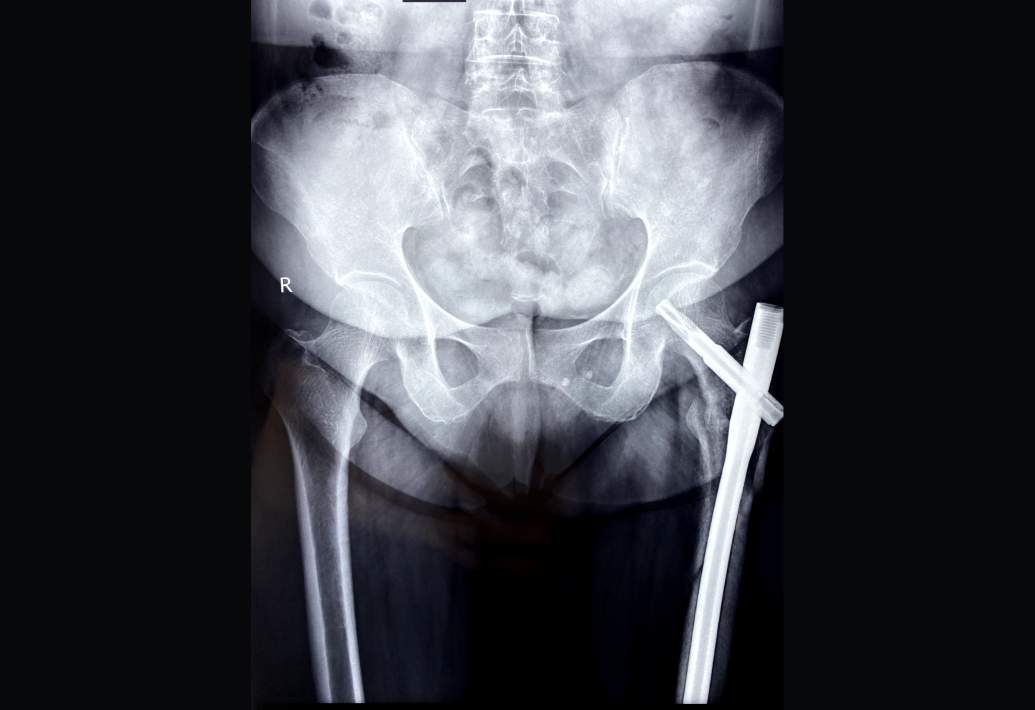
What should I bring to the first consultation?
Bring your medical file, list of current medications, any previous imaging studies (like Xray and MRI) and other relevant reports along with you when visiting the orthopaedic surgeon.
When to consult an Orthopaedic surgeon?
Consult an orthopaedic surgeon if you are suffering from pain, swelling, limited mobility of any joint. Similarly symptoms such as neck pain, back pain, lower limb pain that may or may not be associated with numbness in the hands or feet also warrant an orthopaedic consult. Lastly, if you have suffered an injury then obtain an orthopaedic opinion to rule out bone fractures.
What can I expect in my first orthopaedic consultation?
Your first consult will begin with a detailed history of your symptoms, activity level and past medical/surgical history. At this stage it is imperative to inform the doctor regarding any existing allergies, previous surgeries. After this stage comes the physical examination where the affected limb or part of the body is evaluated to better define the pathology. The patient maybe examined in various positions such as lying down on the examination table, sitting or standing. He or she maybe asked to walk within the room to recognise specific walking patterns. Although the examination is as gentle as possible, slight pain might occur while eliciting certain tests. Next, any existing reports/Xrays/blood tests are screened and discussed with the patient. Additional tests maybe advised as per the need. Lastly, a treatment plan that is tailored to the specific needs of the patients is designed and discussed with the patient. This may include activity modification, application of ice or hot fomentation, use of oral medications, referral to physiotherapist for rehab, use of certain braces or splints and if required then surgery. The doctor will also advise regarding when to schedule a follow-up visit. It is a good idea to carry a list of any potential questions or doubts that you may have for a more comprehensive discussion.